#2020Trends: Care Delivery Model Innovation
I’m back with the third installment in my new blog series on 2020 Trends in Healthcare! Last week, I focused on the retailization of care and how the pressure to manage costs and meet higher patient and consumer expectations is pushing care out of traditional settings. That drive for alternative ways to access care extends into what I see as another big trend for 2020: Innovations in care delivery models.
With advancement in digital healthcare technology enabling easy consumer access, improvements in early diagnosis, application of behavioral science to engage consumers and team-based delivery models with PCP as the quarterback, I expect care delivery models to continue to evolve in 2020. What we’re seeing now speaks to a market that is more engaged and responsive to changing consumer expectations and the drive for more holistic solutions. For example, certain models are putting more emphasis on social determinants that impact consumer health on a broader scale. No longer passive and more willing to engage in preventive behaviors than in the past, consumers are proving more receptive to models that reward commitments to exercise and healthier dietary choices. This pressure from multiple directions is ultimately pushing the care delivery model to change from sick-care to a more proactive focus on well-care.
217 Billion Reasons to Focus on Well-Care
According to research from the Milken Institute, treatment costs for avoidable chronic conditions are expected to reach $217.6 Billion by 2023.
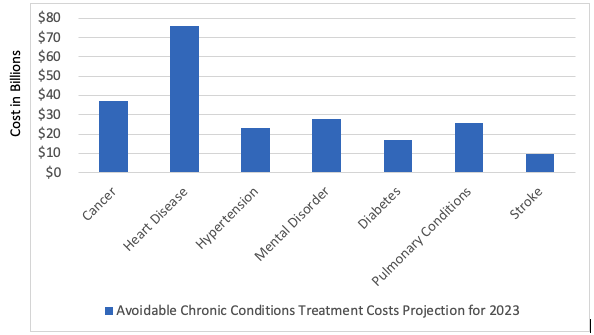
By helping members become healthier, managing their chronic conditions and preventing the onset of sickness and disease in the first place, payors face lower risk of incurring expensive costs while awarding higher reimbursements to providers as a result of better outcomes under value-based care regulations. It’s a true (and rare) win-win for everyone! It’s also a massive paradigm shift.
Moving from a care delivery model focused on sickness to one that instead prioritizes well-care calls for a massive redesign in the way healthcare works for all stakeholders. Providers will need to continue to redesign their care delivery model to align the services they offer and the team that delivers them with the new focus on well-care. It will mean spending more time with patients, timely coordination of care—from primary care to specialist to nutrition support to physical therapy—and keeping health issues in front of the right provider.
Digital Healthcare Innovation
One way the market is responding to this trend is with a highly visible leap into innovations in digital healthcare. VC funding for startups in the digital health space has exploded and will continue to expand as technology like AI powered chatbots, video visits, teleconferences and physician access to data via connected devices are scaled up via new players like Doctolib, Babylon Health and WeDoctor. These high-tech entries into the digital health space are poised to make healthcare more accessible and will continue to change the care model as we know it.
Factoring in Social Determinants of Health
At this point, it is increasingly clear that social determinants of health—factors apart from clinical data and medical history—have an outsized effect on overall health and outcomes. In fact, medical care is now estimated to account for only 10-20% of the modifiable contributors to healthy outcomes. As much as 90% then rests on a combination of health-related behaviors, socioeconomic and environmental factors known as social determinants of health.
So, in a world where a person’s zip code is now a better predictor of his or her overall health than nearly any other factor, an increasing number of US health systems and commercial payors are looking for new ways to utilize social determinant data of some type in making risk assessments, guiding patient outreach efforts and designing new models of care that account for the impact of this reality.
A new program from Denver Health serves as an example of the kind of innovation we’re likely to continue to see develop around social determinants data. In partnership with the Denver Housing Authority, they recently converted a shuttered 10-story building on their campus into affordable senior housing to transition homeless patients out of the hospital. A case manager is also provided to assist with ongoing physical and behavioral health needs of residents. In addition to satisfying the legal and moral obligations of the hospital, the program also works to simultaneously minimize costs and improve outcomes for this high-risk population.
Any Guesses About Trend #4?
Think you know what’s coming up next? Take a guess in the comments! OR cut to the chase and check out my full, on-demand webinar on 2020 trends right now.