Mapping Out MACRA (Part Two)
In the first post of this series we talked a bit about MACRA, its origins, and what it might mean for you. In this post, we are going to break down two key components of MACRA: MIPS and APMs.
UNDERSTANDING MACRA: MIPS vs APMs
The first thing you need to know about MACRA is that there are two basic options for participation: The Merit-based Incentive Payment System (MIPS) and the Alternative Payment Models (APM). Most practitioners will be subject to MIPS, so we’ll start there.
Merit-Based Incentive Payment System
Clinicians who will be included in MIPS are physicians, physician's assistants, nurse practitioners, clinical nurse specialists and certified registered nurse anesthetists (the list of eligible professional will likely expand in 2021). The three forms of MIPS exemptions for clinicians who would otherwise meet the eligibility requirements are the following:
- Clinicians in their first year of Medicare Part B participation
- Clinicians in entities sufficiently participating in an Advanced APM (more on this later)
- Clinicians billing Medicare Part B up to $90,000 in allowed charges OR providing care for up to 200 Part B patients in one year
Note: Originally the threshold for billing was $30,000 and number of patients was 100 but CMS
adjusted this measurement in an attempt to reduce the reporting stress on small practices.
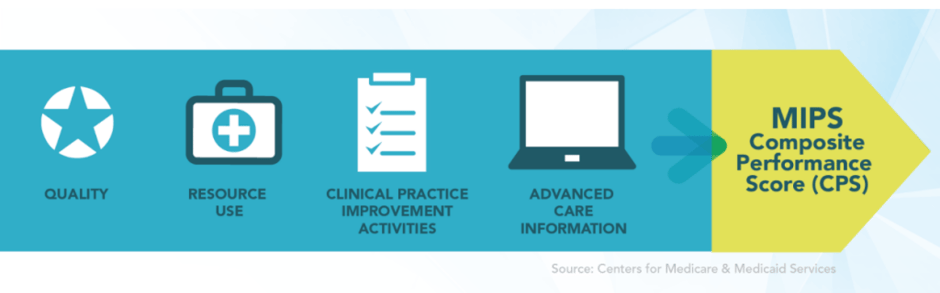
The MIPS Composite Performance Score (CPS)
MIPS reimbursement is based on a composite performance score (CPS). It’s important to take the time to understand the basics on how this is calculated, especially because MIPS allows for a certain level of flexibility for clinicians to choose measurements that are most meaningful to their practice.
In short, MIPS combines and streamlines three existing federal reporting programs:
- Physician Quality Reporting System (PQRS)
- Value-based Payment Modifier (VBM)
- Medicare Electronic Health Record (EHR)
It will also include a fourth category in the calculation called “Clinical Practice Improvement Activities (CPIA).” These “four statutory pillars” are what make up the CPS metric and determine whether an eligible professional will receive a payment bonus, a penalty or no adjustment at all.
 The Quality Score
The Quality Score
The quality category is largely based on PQRS though the number of measures to report will drop from 9 to 6. One measure chosen by the clinician must be outcome based (or high-value) and one must be a cost-cutting measure. The Quality category will have a 60% weighting for the first and second performance year so it is worth the effort to become familiar with the measures you can choose from to make sure you are reporting on the highest potential performance measures.
The Resource Use Score
The Resource Use category replaces the Value-based Modifier (VM) and was originally proposed to have a weight of 10% in a participant’s CPS metric. This category was then simplified and weighted to zero for performance year 2017 and 2018 to allow clinicians to improve their understanding of the measures and ease into the Quality Payment Program.
It’s important to note that CMS states that their intent is to adjust the weights to “align cost measures with quality measures over time in the scoring system.” Which means that we may see that both quality and cost each account for 30% of the CPS in 2019.
The Clinical Practice Improvement Activities Score
Clinical Practice Improvement Activities (CPIA) is a new category and will have a weighting of 15% of the overall CPS. CMS stated in its June 30th proposed rule that “improvement activities are those that support broad aims within healthcare delivery, including care coordination, beneficiary engagement, population management, and health equity.” This category requires a selection of one CPIA activity (from 90+ proposed activities) with additional credit for more activities.
Advancing Care Information Score
The Advancing Care Information is similar to Meaningful Use (MU) and has a weighting of 25% of the CPS. It is focused on interoperability and information exchange and measures how well you are making “meaningful use” of your Electronic Health Records (EHR). One metric in this category will be measured by the use of a Certified EHR technology (CEHRT) “to support patient engagement and improved healthcare quality” and CMS recommends that physicians and clinicians “migrate to the implementation and use of EHR technology certified to the 2015 Edition” but they have recognized the challenges some may have in adopting new certified IT and proposed that clinicians may continue to use 2014 edition CEHRT for the 2018 performance year. That said, as an incentive to still make the change next year, providers who do use the 2015 Edition would receive a 10 percent ACI bonus.
Payment Adjustment Range
MIPS reimbursement is dependent on how your overall Composite Performance Score (CPS) stacks up against the MIPS performance threshold.
The adjusted payments will start at plus or minus 4 percent in 2019 and incrementally increase to 5 percent, 7 percent and then 9 percent in 2020, 2021 and 2022, respectively.
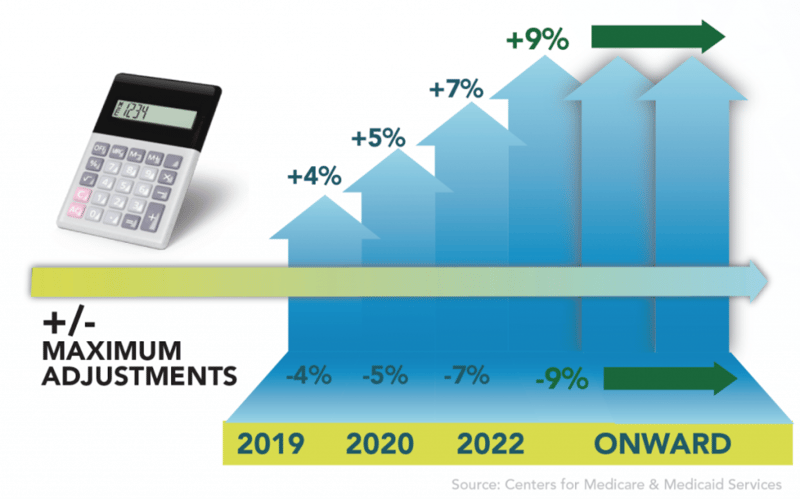
There will also be a 3 times multiplier bonus available for those who achieve the 25th percentile. Therefore, by 2022 your MIPS score could earn you a 27% adjustment increase, or conversely you could lose up to 9% of your reimbursement for performing poorly.
ALTERNATIVE PAYMENT MODELS
The other option under MACRA is the Alternative Payment Models (APM) which include Accountable Care Organizations (ACOs), Medicare Shared Savings Programs and Patient-Centered Medical Home models (PCMH). A clinician may join an existing APM entity or apply to CMS to create a new APM entity. In order to create a new APM entity, one must adhere to the application procedures and deadlines published by CMS.
Because APMs provide a wide array of participation options, it is important to review the variety of APMs that are available. Before a new APM is published by CMS, they decide whether the model satisfies the requirements for a ‘MIPS APM,’ a ‘Medical Home Model,’ a ‘Use of CEHRT Criterion,’ a ‘Quality Measures Criterion,’ a ‘Financial Risk Criterion,’ or an ‘Advanced APM.’
For a list of approved Advanced APMs for the 2017 performance year visit:
https://qpp.cms.gov/docs/QPP_Advanced_APMs_in_2017.pdf
Up Next
In our next installment we will discuss the key factors to consider when deciding which path would be best for you and your practice. This post will include pros and cons for both MIPS and APMs, has guidance regarding data strategies, and has guidance on change management strategies as well. Stay tuned for that post, or go straight to the source and get the full story right now!